The rate of infertility is nearly equal between sexes before middle age, yet women still bear the brunt of society’s pressure.
 Male infertility is common and does not discriminate based on wealth or geography.
It is the unspoken canary in the coalmine of male health. (Stock image) : Jakob Owens via Unsplash (https://unsplash.com/photos/man-in-black-jacket-sitting-on-bed-98PkChn547Q) Unsplash Licence
Male infertility is common and does not discriminate based on wealth or geography.
It is the unspoken canary in the coalmine of male health. (Stock image) : Jakob Owens via Unsplash (https://unsplash.com/photos/man-in-black-jacket-sitting-on-bed-98PkChn547Q) Unsplash Licence
The rate of infertility is nearly equal between sexes before middle age, yet women still bear the brunt of society’s pressure.
Almost exactly a year ago, the eight billionth person was born, apparently in the Philippines. In just 11 years, the world had added a billion people to the population.
It might sound bizarre then, to learn that there is a worldwide fertility problem.
The fact is in the last 60 years, the global birth rate has dropped from 5.3 to 2.3 births per woman. This is seen by many as a product of modern life, where couples choose to have fewer children later in life. Such choices are valid and have contributed to improved economics and health of many, notably women and children, across the globe.
That narrative is false.
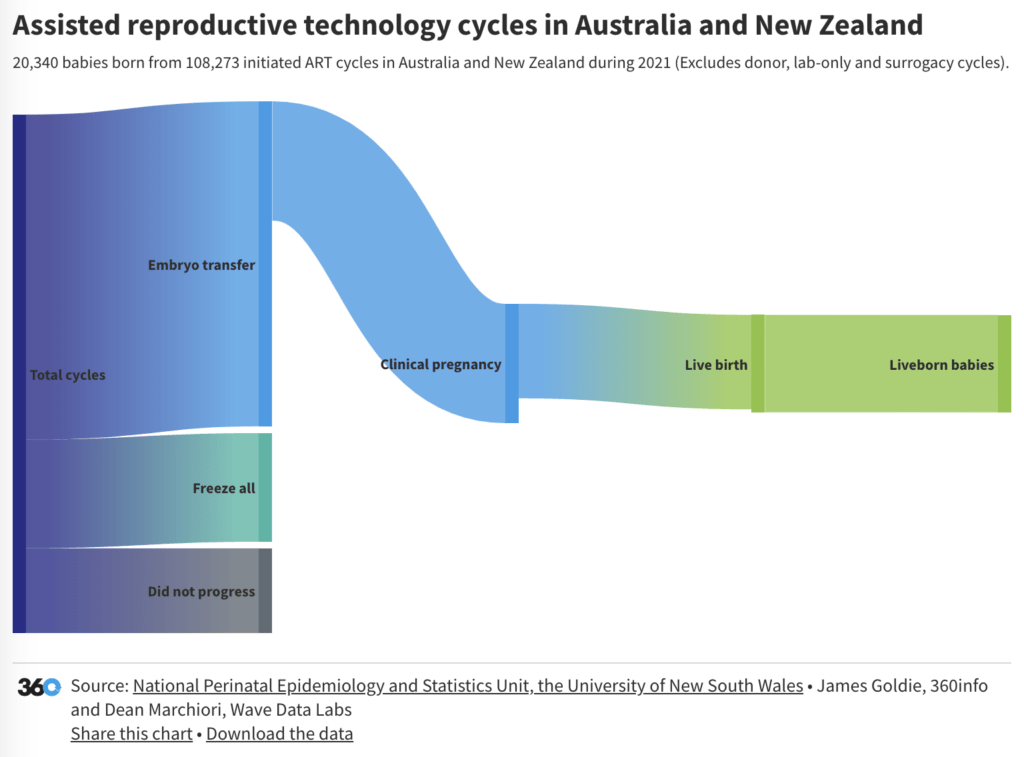
The blanket perception of ‘choice’ hides the reality that the World Health Organization estimates that 1 in 6 couples are in fact infertile. In April, a WHO report claimed that an estimated 17.5 percent of the adult population is infertile and that number is increasing yearly.
Perhaps more surprisingly to many the incidence of infertility between sexes is almost equal— estimated 35 percent of the time due to women and 30 percent due to the male, with the remainder due to a combination or unknown causes.
Male infertility is common and does not discriminate based on wealth or geography.
It is the unspoken canary in the coalmine of male health.
Compounding this is the failure of health systems to recognise the burden of male infertility at a more significant level and the potential that infertility may be caused by or be a marker of other illness.
For most men, the cause will remain unidentified. Often, this is because there isn’t enough knowledge about the production of the reproductive cells, known as gametes, and how they are affected by environmental and lifestyle factors.
Defining the precise causes of male infertility demands more effort to identify its subtypes. We must move beyond characterising patients based only on semen composition and automatically moving to assisted reproduction which, after all, is a strategy to bypass the problem rather than treat it.
Alarmingly, tests to provide a precise diagnosis of male infertility are rare, and consequently, few targeted treatments exist.
Unlike many areas of health, DNA or genome sequencing is not currently standard practice – and even if it was, researchers are yet to develop the tools to read the genetic map of how to produce functional sperm. Research into achieving such knowledge is essential.
Each man entering into medically assisted reproduction without a thorough consideration of the potential causes of infertility and co-morbidities is a missed opportunity. Furthermore a woman with no identified reproductive disease or history often becomes the patient to ‘treat’ a presumed male fertility issue.
This highlights the inherent gender inequity in the approach to infertility treatment. Procedures are performed on women when it’s men’s infertility that may be the problem.
The misnomer of ‘treatment’ for male infertility is emotionally taxing for the man and woman and involves considerable time and financial commitment. It is also invasive and includes a risk to the woman’s health.
The failure to identify precise causes of male infertility at a molecular level, also means that few real treatments exist.
This inequity works both ways, by circumventing male infertility as a problem it denies treatment of the underlying medical for the individual and further pushes community awareness of the growing portion of the population going through the same situation further from the surface. This is in spite of the fact that evidence suggests that men are searching in greater numbers for the cause of their infertility.
There are multiple complex reasons why people experience infertility, almost certainly involving a mix of biological changes, environmental and lifestyle exposures.
A roadmap for governments, society and health bodies, to change the conversation surrounding fertility, could work to address the current level of concern and ultimately provide real treatments for the benefit of men, their partners and their children.
First, the simple goal could be that all parties need to acknowledge male infertility is a common, serious medical condition, and patients have a right to meaningful diagnoses and targeted treatments.
Equally, the bodies controlling public health funding could establish a global network of registries and biobanks containing standardised clinical and lifestyle information linked to national healthcare data systems for testing so as to unpick those sub-types of infertility caused by genetic changes, environmental insults, or an interaction between the two.
Potentially environmental causes may be removed by governments or individuals. Importantly, such databases should encompass a wide geographic distribution.
With the identification of precise molecular causes of male infertility, true treatments may be developed.
Agencies can implement regulations to ensure the rigorous testing of compounds for adverse effects on male fertility and the sharing of results globally – notably, and urgently, around classes of compounds known as endocrine disrupting compounds.
In parallel, regulatory policies that control the use of compounds that alter reproductive health in products, the workplace and the environment could be enacted while investing in research to develop safe chemical alternatives.
Society at large could normalise the conversation around male infertility to encourage action to achieve these formidable goals.
Normalisation comes through education and public health campaigns, where infertility becomes recognised as a common, serious and urgent disease.
Ideally, such campaigns should be lifelong, easily understandable, accessible and linked to healthcare systems through improved and continuous education of the healthcare workforce in the broad area of male reproductive health.
The training for the industry could be emphasised during medical school, providing ongoing training and resources to health professionals integrating services across urology, internal medicine, endocrinology, gynaecology and paediatrics.
The task is considerable, but the public is not starting from zero. Many laboratories have made impressive advances. Adopting new sequencing technologies is already revealing a rapidly expanding number of genetic causes of human infertility.
Success in research leads to the treatment of male reproductive disorders, and through implementation into standardised global healthcare practices, men, their partners, and future generations will live long and healthy lives.
Professor Moira O’Bryan is a professor and Dean of the Faculty of Science at The University of Melbourne. The focus of Dr O’Bryan’s research is sperm development and function, genetic and environmental causes of human infertility.
Professor Robert McLachlan is the Adjunct Professor at Monash University based at the Hudson Institute – Centre for Endocrinology and Metabolism. He is Consultant Andrologist to the Monash IVF Group and Medical Director of Healthy Male, a Federal Government Department of Health supported educational activity in male reproductive health.
Originally published under Creative Commons by 360info™.