To make infertility care widely accessible, services for basic infertility investigations can be integrated into existing reproductive health facilities.
 Advanced fertility treatment should be accessible and affordable to less privileged groups. : Anurag Gautam Unsplash
Advanced fertility treatment should be accessible and affordable to less privileged groups. : Anurag Gautam Unsplash
To make infertility care widely accessible, services for basic infertility investigations can be integrated into existing reproductive health facilities.
There is an idea in developing nations that infertility doesn’t need to be the focus of family planning programmes because of “overpopulation”.
In India, the world’s most populous nation, this idea has taken hold, meaning childless couples — especially in rural areas or from less privileged backgrounds — find it difficult to seek treatment.
The irony is, Assisted Reproductive Techniques (ARTs) are increasingly available to foreigners or those with the money to afford them.
Contrary to the population policies of developing countries, which focus primarily on reducing total fertility rates, research says infertile couples must have access to ARTs despite the state’s fears that contributing to demographic growth in this manner would result in further overpopulation.
Denying infertility treatment is an ill-considered population control policy.
Unlike in developed countries, where couples increasingly opt to not have children, in India involuntary childlessness could be treated as an important reproductive health and rights issue.
In India, a few districts are underperforming in terms of fertility treatment received by women. There have also been increasing cases of male infertility in the post-COVID era and reduced fertility rates in south Indian states like Kerala, Tamil Nadu, Karnataka and Telangana.
The management of infertility requires prioritising certain public health concerns in India.
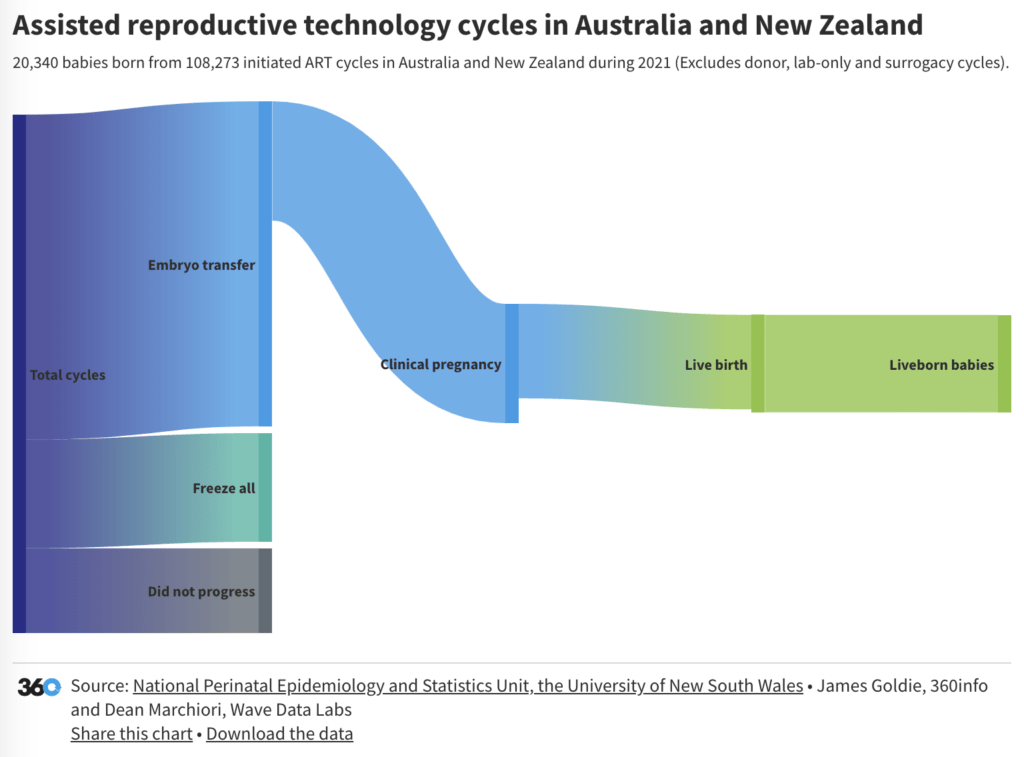
The advancement in treatments such as in-vitro fertilisation (IVF) has improved assisted births, opening the doors not only to many Indian couples who have been struggling with infertility for years but to many couples from other countries.
Medical tourism is booming due to the cheap ART and IVF facilities offered to international patients in India as compared to the US, UK and Singapore. India offers a significantly lower price range of USD$1200 to USD$2500 per IVF cycle.
Experienced medical personnel, pre- and post-procedure provisions and reduced language barriers have made India a favourable destination for medical tourism in IVF.
The country currently sees up to 250,000 IVF cycles per year. The future looks promising as the Indian fertility industry has grown 20 percent in the last five years and is expected to grow at the same pace in the next five years.
Still, infertility treatments are very costly and sometimes lead to out-of-pocket expenses or catastrophic health expenditure for those who need it, as they spend a greater proportion of their income on fertility care compared to people in wealthier societies. ARTs are mostly inaccessible for most couples in developing countries like India.
Families from low- and medium-income groups still can’t afford IVF. The costs incurred by couples from rural areas are relatively higher than those from urban areas, regardless of the type and phase of treatment consulted. Rural couples are forced to visit urban fertility clinics for treatment and to bear the travel expenses for food, transport, accommodation and other expenses.
A 2022 study in rural West Bengal explored that a considerable proportion of couples could not opt for advanced allopathic fertility treatment due to its high cost. Couples stop their treatment for many reasons although cost and inaccessibility are the most common.
Inaccessibility due to lack of transport, lack of knowledge about available treatment options and lack of diagnostic facilities at the primary health centres in rural areas are the other factors that make fertility treatment inaccessible to poor people.
As a result, despite their inclination towards modern treatment, some couples seek varied low-cost traditional methods and religious practices in rural areas.
The demand for infertility medical services and ARTs varies, driven mostly by the couple’s socio-economic background.
Disparities in access to treatment may lead to additional disparities in health and quality of life. The West Bengal study shows that about 54 percent of women diagnosed with infertility in rural areas took a long time to realise the necessity of fertility treatment and spent a long time seeking this treatment due to lack of information, counseling and proper knowledge of reproductive health problems such as pelvic inflammatory disease, endometriosis or polycystic ovary syndrome.
If the causes of infertility problems are diagnosed early, treatment becomes easier.
It is necessary to make ARTs accessible and affordable to less privileged groups.
To make infertility care widely accessible, services for basic infertility investigations to determine the cause of infertility and simple forms of infertility treatment such as ovulation induction and artificial insemination could be integrated into existing reproductive health programmes.
Sallam’s model of fertility assistance may be effective in a rural context, consisting of a basic infertility clinic offering diagnostic tests and simple forms of infertility treatment; an advanced clinic where IVF, the simplest procedure and more advanced diagnostic procedures are available in addition; and a tertiary-level infertility clinic offering specialized assisted reproduction and surgical procedures.
In rural India, women with higher levels of reproductive health knowledge, which correlates with their level of education, are more likely to receive allopathic treatment for infertility whereas those with low reproductive health knowledge tend to opt for traditional, superstitious or religious treatments.
The role of low-cost treatment alternatives like ayurveda, yoga and naturopathy, unani, siddha and homoeopathy or Ayush needs to be assessed thoroughly.
India’s commitment to comprehensive reproductive health service delivery can emphasise the awareness of fertility and the factors affecting it.
In addition to public services, the private sector and the traditional healer are both important alternative sources of first help in rural areas. The involvement of healthcare staff from both the formal and informal sectors when investing in the education of infertile couples and the community is important.
One of the targets of the United Nation Sustainable Development Goal 3 is to ensure universal access to sexual and reproductive healthcare services by 2030. Maternal health starts with quality reproductive health care that includes pre‐conception fertility care.
In India, no medical insurance covers the medical expenditure on infertility treatment.
Arguments for mandatory insurance coverage may let the government enact regulations that require varying forms of insurance coverage for infertility treatment.
Dr. Shraboni Patra is a Women and Child Health Researcher at Centre for Technology Alternatives for Rural Areas (CTARA), IIT Bombay, Mumbai. She also works with the Public Health Department, Maharashtra, and was earlier at International Institute for Population Sciences (IIPS), Mumbai, India.
Originally published under Creative Commons by 360info™.