Researchers in Sydney have designed a way to bring distance-delivered care to childhood cancer survivors, even in remote settings.
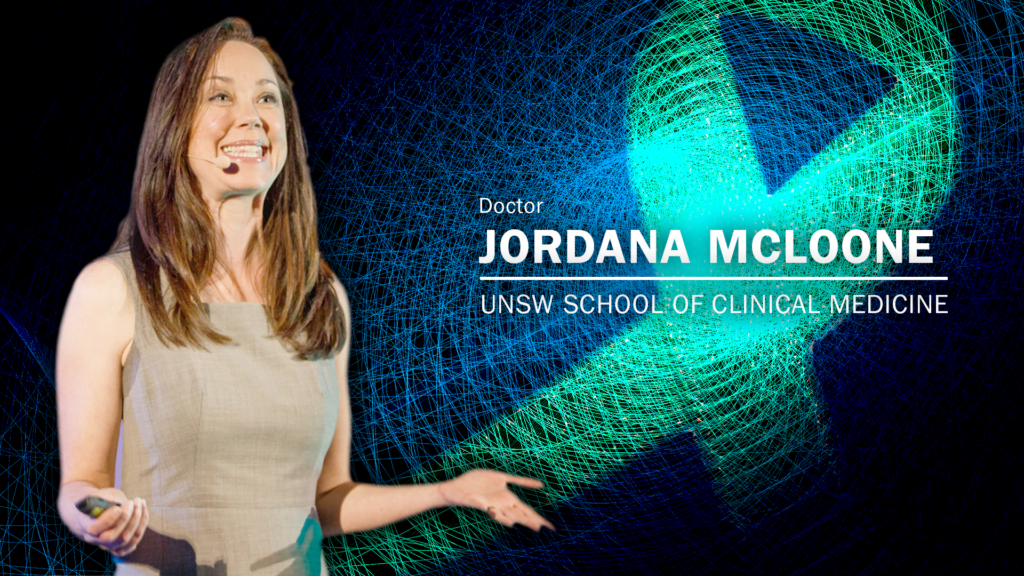 Dr Jordana McLoone, researcher at UNSW Sydney School of Clinical Medicine and the Kid’s Cancer Centre at Sydney Children’s Hospital : Michael Joiner, 360info CCBY4.0
Dr Jordana McLoone, researcher at UNSW Sydney School of Clinical Medicine and the Kid’s Cancer Centre at Sydney Children’s Hospital : Michael Joiner, 360info CCBY4.0
Researchers in Sydney have designed a way to bring distance-delivered care to childhood cancer survivors, even in remote settings.
Transcript:
Quotes attributed to Dr Jordana McLoone, researcher at UNSW Sydney School of Clinical Medicine and the Kid’s Cancer Centre at Sydney Children’s Hospital:
“Over 80 percent of children go on to survive a diagnosis of cancer. Cure is the most probable outcome, and we celebrate this. However, around 95 percent of those children will go on to develop late effects – the long-term side effects of treatment because their treatments are so toxic on their young, developing bodies.”
“It can be a recurrence or relapse. However, quite often it is the development of new chronic illness, such as cardiovascular disease or fertility issues, that develop over time. And we’re talking sometimes 10, 20, 30 years post-cancer treatment completion.”
“However, this is very difficult for a healthcare system to continue to provide care for decades post the treatment of the acute illness. So part of our research we developed personalised health care recommendations for survivors of childhood cancer who had been disengaged from care and provided them to the survivor and their GP [general practitioner].”
“We followed this up over time and on average survivors were given around six health recommendations. Six months later, they could recall two, had adhered to one, and made up a third. We don’t know where they got it from.”
“So now whenever we make these personalised health recommendations, we ensure that we include a booster follow-up session, maybe three months down the track, to help them to ensure that they receive the health education that they need, to know why it is so important for them to continue to pursue these health recommendations, and also troubleshoot any barriers to care, help them navigate the health care system.”
“We knew that our clinics were at capacity, so we were going to have to design an intervention that triaged people to primary care. But we also knew that GPs weren’t confident to manage the care of childhood cancer survivors, nor were the childhood cancer survivors confident in their GP’s management.”
“So we developed Engage, which is a distance-delivered childhood cancer survivorship intervention. The design is that we have developed a very thorough health and lifestyle assessment that systematically works through all of the body systems, as well as mental health, health behaviours, fertility, family history and a number of other things that are very important in understanding their current health needs.”
“So we’ve run two trials of this, a pilot, and in two trials studies. One was all childhood cancer survivors and the other was for brain cancer specifically, since brain cancer often does have those poorer outcomes. We needed to be confident that this could be effective in perhaps one of the trickiest scenarios – especially as it is distance delivered, we wanted to feel really confident that nothing would be missed in in that remote setting.”
“Our studies have included around 200 participants, but that’s the population that we’re having to build the health care system for. Australia has around, child and adolescent survivors. So it’s just a matter of staffing and budgets.”
Dr Jordana McLoone is a Research Fellow and Lecturer with the Discipline of Pediatrics, UNSW Sydney School of Clinical Medicine. She is also a Post-Doctoral researcher at the Kid’s Cancer Centre, Sydney Children’s Hospital, Randwick.
Originally published under Creative Commons by 360info™.
Editors Note: In the story “The state of cancer care” sent at: 01/02/2024 12:12.
This is a corrected repeat.