Cancer puts a huge financial burden on families. Programmes to help cope with the cost can only help patients and their loved ones.
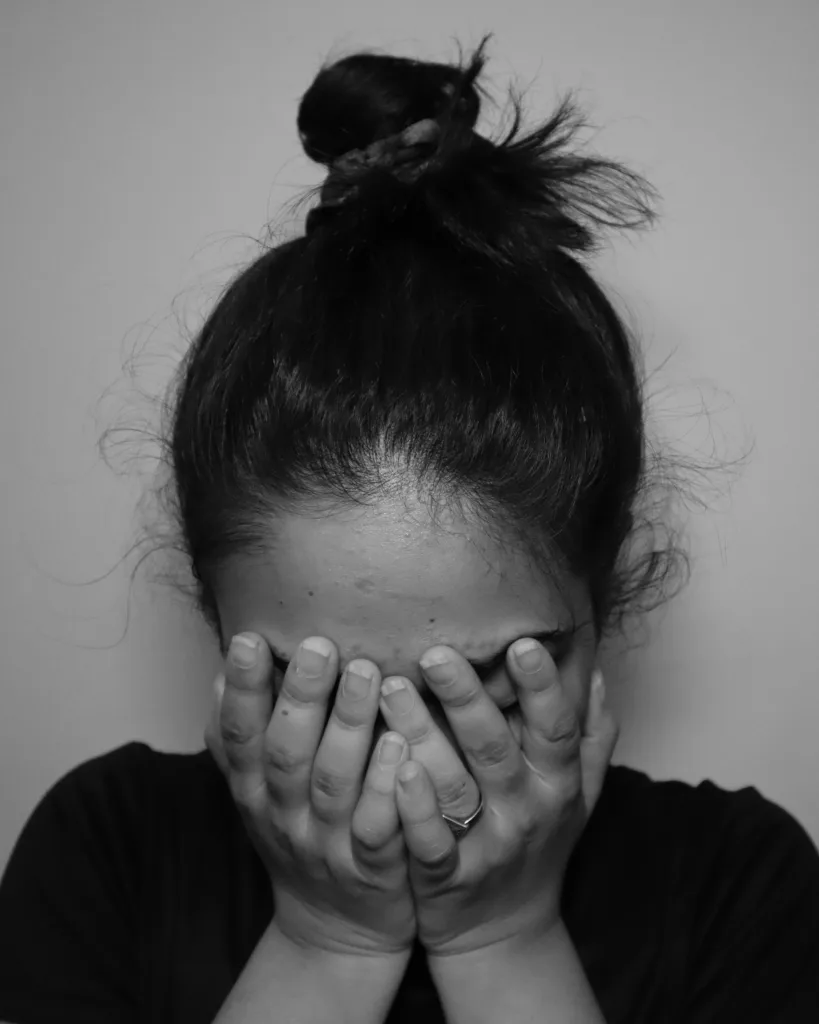 Irrespective of their economic status, people need assistance in understanding the costs of cancer care, filing health insurance claims and accessing financial resources. : Simran Sood Unsplash
Irrespective of their economic status, people need assistance in understanding the costs of cancer care, filing health insurance claims and accessing financial resources. : Simran Sood Unsplash
Cancer puts a huge financial burden on families. Programmes to help cope with the cost can only help patients and their loved ones.
Around one in two households in Southeast Asia with a cancer patient will spend more than a third of their income on treatment.
The ASEAN Costs in Oncology (ACTION) study, involving almost 10,000 cancer-stricken households in eight low- and middle-income countries, showed 48 percent of patients and their families made catastrophic out-of-pocket cancer-related expenditures within a year after a cancer diagnosis.
Apart from the direct medical expenses incurred from diagnostic scans, anticancer therapies, hospital stays and clinical follow-ups, the study found that non-health expenditures such as transport, childcare and household help were important cost drivers that pushed families into debt.
Traditional and complementary therapies are prevalent and deeply rooted in cultural and religious beliefs in Southeast Asia, meaning spending on complementary medicine by people with cancer was associated with the worst financial outcomes, including a higher risk of poverty.
The indirect costs of cancer, such as loss of household income, attributed to pay cuts, job loss and reduced workplace productivity exacerbate the financial burden of cancer.
Cancer patients have also reported experiencing discrimination and stigma, such as being overlooked for a promotion or when applying for a new job, because of their diagnosis.
It’s not only patients. Caregivers reported disruptions to their employment, including having to quit their job or take unpaid time off to care for their loved ones.
Adequate paid sick leave during treatment, flexible work arrangements and time off to attend hospital appointments would help protect the financial wellbeing of patients and their families, as well as facilitate a smooth transition in returning to work.
In Malaysia, an upper-middle-income country with a mix of public and private health providers, the study revealed several important and actionable themes. Besides the costs of anticancer therapies, it’s apparent that the long-term financial burden must also be addressed.
For instance, women with breast cancer who had undergone a mastectomy would require special bras, which can cost from USD$20 to well over USD$100 for custom-fitted pieces. People with colorectal cancer would usually need colostomy or stoma bags after surgery. Simple one-piece systems might cost below USD$10, while ones with advanced features like leak-proof designs can be as high as USD$50 or more.
These supportive care items, and others such as diapers, are often costly and not reimbursable by health insurance. This places a heavy financial burden on patients, particularly those from lower income groups.
Follow-up care is also crucial to monitor and detect a recurrence of cancer, while supportive cancer care enables patients to live and thrive. The costs of these can have serious financial implications and require investigation, including in health insurance reimbursement. This includes countries that have made good progress towards achieving universal health coverage.
While the financial distress following cancer varied largely depending on patients’ socioeconomic status and cancer site, the study found higher-income households and those with private health insurance were also financially affected and had unmet financial needs.
Irrespective of economic status, there was a need for assistance in understanding the costs of cancer care, filing health insurance claims and navigating the complex system in accessing financial resources. A lack of awareness and the tedious paperwork involved in applying for financial assistance were repeatedly highlighted as major barriers.
Families also need more than just help with insurance claims and getting charity assistance.
Financial navigation programmes differ from the traditional and more limited financial counselling programmes by proactively reaching out and developing comprehensive plans to meet each patient’s unique financial needs.
Financial navigation includes assessing risk of financial toxicity — when the cost of cancer care starts to harm a person’s well-being — along with optimising the use of health insurance for medical therapies; connecting patients to available financial resources and helping with paperwork to apply for financial assistance.
Besides reducing financial toxicity due to treatment costs, financial navigators may also help alleviate non-medical financial stressors such as childcare, food and mortgages by connecting patients with available community services and resources.
Such programmes, however, are scarce in the low- and middle-income countries, where the financial burden of cancer may be exacerbated by poorer social welfare services.
To this end, financial navigation programmes may serve as a bridge to not only connect patients to financial resources, but also facilitate these connections by streamlining application processes and paperwork.
Nirmala Bhoo-Pathy is a professor at Universiti Malaya, who strives to improve life after cancer, particularly for families in low- and middle-income countries. Leading major studies like ACTION, she equips policymakers with evidence to reduce cancer’s financial burden and save lives. Dr. Bhoo-Pathy’s dedication extends beyond research, as she actively champions the needs of cancer patients through influential global roles.
Yek-Ching Kong, an epidemiologist and Research Associate with Well with Cancer @ Malaysia (WeCan@MY) research group at Universiti Malaya, delves into the financial and economic complexities of cancer in low- and middle-income countries (LMICs). Her research aims to unlock solutions for improving patient-centered outcomes after cancer, focusing on areas like financial toxicity and healthcare access in these resource-limited settings.
Disclosure statement
NB-P reports receiving grants or contracts from Novartis, Pharmaceutical Association of Malaysia, Pfizer, Roche and Zuellig Pharma and, outside of the submitted work. NB-P also reports receiving payment or honoraria for lectures, presentations, speakers bureaus, manuscript writing, or educational events from Novartis, Pfizer, Roche and Zuellig Pharma; receives support for attending meetings or travel from Novartis, Roche and the Pharmaceutical Association of Malaysia; reports participating on a Data Safety Monitoring Board or Advisory Board with Zuellig-Pharma, Malaysia; reports leadership or a fiduciary role in other board, society, committee, or advocacy groups, paid or unpaid with the National Cancer Society Malaysia, and eCancer and is the Associate Editor of the Psycho-Oncology journal outside of the submitted work.; and reports receipt of equipment, materials, drugs, medical writing, gifts, or other services from Roche Diagnostics, all outside of the submitted work.
Originally published under Creative Commons by 360info™.