Cancer cachexia affects 50 to 80 percent of people with cancer, but you may never have heard of it.
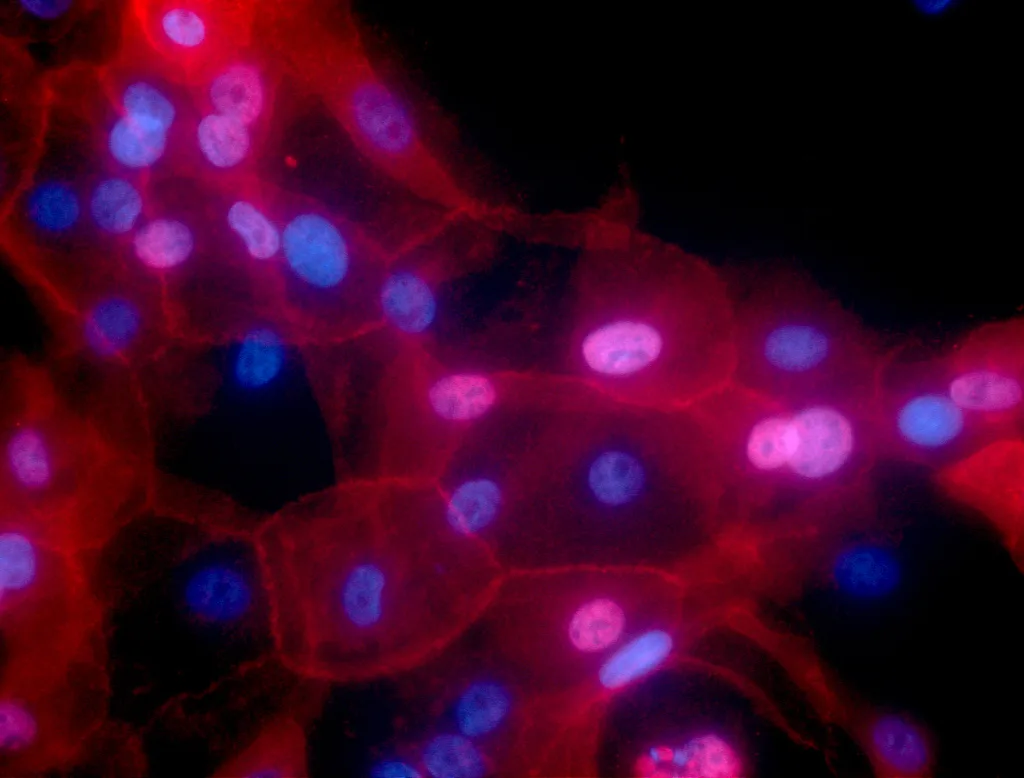
 Cancer cachexia can lead to unintentional weight loss, loss of muscle strength and fatigue. : Unsplash: National Cancer Institute Unsplash Licence
Cancer cachexia can lead to unintentional weight loss, loss of muscle strength and fatigue. : Unsplash: National Cancer Institute Unsplash Licence
Cancer cachexia affects 50 to 80 percent of people with cancer, but you may never have heard of it.
“Wasting away”, “looking starved” or feeling a loss of self are just some of the ways people describe themselves or their loved ones living with cancer cachexia.
Cancer cachexia is a pervasive but often overlooked condition that affects 50 to 80 percent of people with cancer.
Despite its prevalence, the condition often goes unrecognised, leaving patients and even healthcare providers grappling with its elusive nature.
Often confused or conflated with the side effects of treatments such as chemotherapy, cachexia is usually associated with unintentional weight loss, loss of muscle strength and fatigue. Reduced appetite, changes to taste and nausea are also common symptoms.
But awareness of the condition is increasing, alongside understanding of how it might best be managed.
Unlike starvation, where feeding more calories leads to weight regain, cancer cachexia is a complex web of factors — including inflammation, changes in the way the body produces or maintains energy, and the body’s response to the presence of cancer cells — all of which contribute to muscle breakdown.
This complexity has made finding treatments difficult, with no ‘silver bullet’ in the form of a single medication.
The silent progression of cachexia can be particularly insidious, reducing the effectiveness of anti-cancer treatment and the overall wellbeing and quality of life of people with cancer.
Recognising cachexia as a separate condition allows healthcare professionals to tailor interventions that aim not just to treat the cancer but also to mitigate the debilitating effects of cachexia on a person’s overall health.
While a definitive cure remains elusive, effective management strategies can significantly reduce its impact and improve patient wellbeing.
A multidisciplinary approach is proving to be a crucial component in addressing this multifaceted condition. It involves healthcare professionals such as palliative care specialists, oncologists, nurses, dietitians, physiotherapists and mental health specialists, as well as patients themselves.
The approach usually includes four main elements:
Nutritional support
Ensuring adequate nutritional intake is a cornerstone of managing cancer cachexia.
Dietitians may work closely with patients to tailor nutrition plans that not only meet their caloric needs but also address the specific nutritional challenges posed by cancer and its treatments.
Often this includes high-protein and high-calorie food. Nutritional supplements may be recommended to bridge nutritional gaps and support overall wellbeing.
Exercise programs
Physical activity has shown promise in countering muscle wasting and improving overall strength and functionality, and providing a sense of regaining control.
Tailored exercise programs developed with a physiotherapist or exercise physiologist can be adapted to a patient’s capabilities and can contribute significantly to the management of cancer cachexia.
Pharmacological interventions
Several drugs are being investigated for their potential in mitigating cancer cachexia, though their wide use has not yet been approved in any country except Japan.
These include appetite stimulants, anti-inflammatory agents and drugs targeting specific pathways involved in muscle wasting.
Rather than curing cachexia, the focus of these drugs is more often on controlling symptoms such as nausea, lack of appetite and pain. While no single medication has emerged as a definitive solution, ongoing research holds promise for future breakthroughs.
Psychosocial support
Mental health and wellbeing play a vital role in managing cancer cachexia, both for patients and those who care for them.
Doctors, nurses and mental health professionals assist patients in coping with the emotional toll of their condition, addressing anxiety, depression and the psychological impact of significant weight loss.
They may also help families and loved ones with the stress and conflict that may come up during this time.
This holistic approach recognises that managing cachexia extends beyond the physical realm, encompassing mental and emotional wellbeing.
Research has underscored the benefits of adopting a multidisciplinary and shared decision-making approach in tackling cancer cachexia.
A collaborative effort ensures that healthcare professionals pool their expertise to tailor interventions to each patient’s unique needs.
Shared decision-making involves patients actively participating in their care, providing them with a sense of agency and encouraging them to take control of their treatment plans.
The benefits of taking a multidisciplinary and shared decision-making approach extend beyond mere symptom management.
Studies have indicated that such collaborative efforts result in improved treatment tolerance, reduced hospitalisation rates and an overall enhancement in the patient’s ability to withstand the challenges of cancer therapies.
Studies show that patients engaged in shared decision-making processes are more likely to stick with nutritional and exercise recommendations, leading to improved outcomes.
Moreover, a collaborative approach enables early identification of cachexia, allowing for timely intervention and a more effective management strategy.
Future research endeavours must focus not only on unravelling the intricate mechanisms underlying cachexia development, such as identifying biomarkers and therapeutic targets, but also on ways to make supportive cancer care accessible for people with cancer.
Clinical trials exploring novel interventions, such as pharmacological agents and targeted therapies, are vital for expanding the toolbox for cachexia management.
Large-scale community-based studies can provide valuable insights into the prevalence and risk factors associated with cachexia, guiding the development of preventive strategies.
The future of cachexia research hinges on collaborative efforts between clinicians, researchers, patients and the broader community.
Increasing awareness, fostering a commitment to continued research and advocating for shared decision-making will contribute to more effective interventions.
By empowering patients to actively participate in their care, the gap between scientific knowledge and the human experience can be bridged, ultimately improving the lives of those affected by cancer and cachexia.
Dr Vanessa Vaughan is Sub-Dean for Global Medicine at the University of Western Australia. Their research focuses on the way people interact with and experience health services, particularly improving outcomes for people with cancer cachexia by applying evidence-based interventions in person-centred care.
Originally published under Creative Commons by 360info™.