Sixty healthy volunteers took magic mushrooms in a lab, and scientists recorded their brains during their experience.
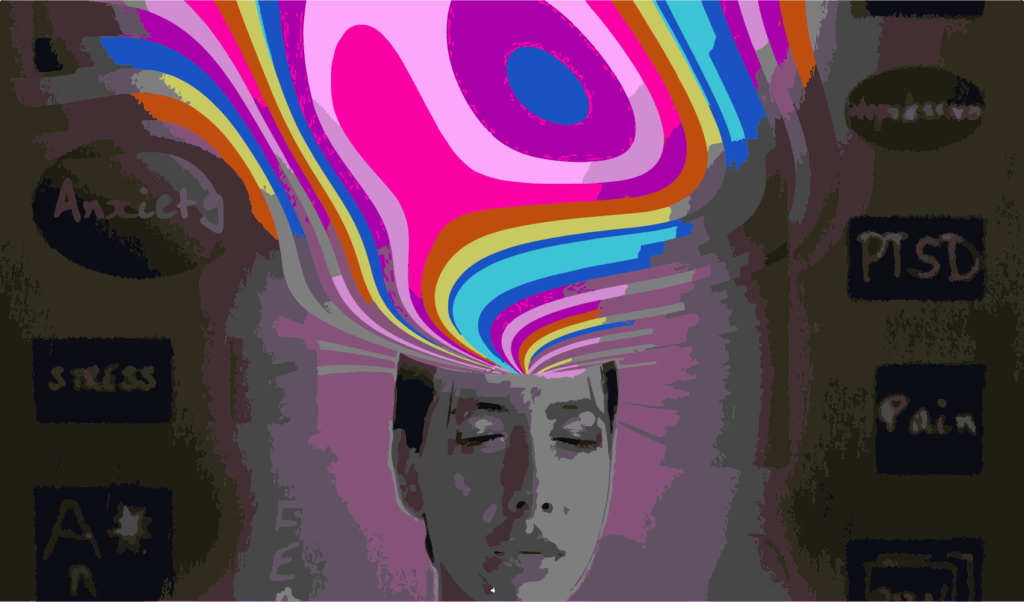
 PsiConnect is the first imaging trial of participants on psychedelics in Australia. : Dmitriy Gutarev/Pixabay Pixabay License
PsiConnect is the first imaging trial of participants on psychedelics in Australia. : Dmitriy Gutarev/Pixabay Pixabay License
Sixty healthy volunteers took magic mushrooms in a lab, and scientists recorded their brains during their experience.
Approximately half of the Australian population will experience a mental health disorder during their lifetime, and scientists are turning to an unlikely place in the search for treatment.
Researchers at Monash University are scanning the brains of healthy adults under the influence of psychedelic drugs. They aim to identify the pathways in the brain that underlie the effects of these substances to build an understanding of how different parts of the brain are connected in general. PsiConnect (comprising Psilocybin, Connectivity and Context) is the first imaging trial of participants on psychedelics in Australia, and with 60 participants, is one of the largest psychedelic imaging trials worldwide.
Many kinds of psychedelics exist, derived from different plants, animals, and fungi. When a person takes a psychoactive substance, there is a temporary reorganisation of brain connectivity that alters perception. It can cause hallucinations and can change self-perception.
Counter-intuitively, psychedelic-induced distortions of perception can have a positive effect in clinical patients with dysfunctional forms of thinking — such as self-limiting beliefs and pervasive pessimism. By temporarily deconstructing perception in the context of therapy, psychedelics may help people find alternate ways to improve their self-perception and belief. It is these changes that have reinvigorated interest in the therapeutic potential of psychoactive substances.
While some researchers argue that psychedelic therapeutic effects derive from the experience of altered consciousness, others suggest this may not be the case and seek to separate the therapeutic effects from the psychoactive experience. It may be that both the non-psychoactive properties and psychoactive properties of these substances contribute to their therapeutic effectiveness.
However, before psychedelics are used to treat a specific mental health diagnosis, some potential problems need to be considered. For example, psychedelics may be harmful to people who have a genetic predisposition to psychosis. Rigorous scientific study is needed if psychedelics are to be integrated into publicly available therapy in a realistic, safe and lasting way.
At the Monash University Computational Neuroscience Lab, the ongoing psychedelic imaging trial uses synthesised psilocybin — the magic ingredient in ‘magic mushrooms’ — supplied by Usona Institute, a medical research organisation. The trial uses a fixed dose of 19 mg, an amount based on prior studies and recommendations of researchers, to reliably create the psychedelic effects of psilocybin at a level that is generally well tolerated by healthy adults, regardless of gender or body weight.
Participants have two sessions of brain scans at the Biomedical Imaging facility at Monash, one before and one after the psilocybin. They take the drug as a pill in a comfortable non-clinical setting at the Turner Institute’s BrainPark, in the company of the researcher, study doctor and support staff. Most people start feeling the effects of psilocybin about an hour later, so scanning begins.
First, functional magnetic resonance imaging (fMRI) takes high-resolution pictures of the whole brain, including deeply located subcortical parts, and measures how that activity changes over time. The researchers also use an electroencephalograph (EEG) after the MRI, because it can measure millisecond changes in brain connectivity, although with much lower (spatial) resolution.
The study also investigates how context plays a role in the effects of psilocybin, by providing different music as the scanning takes place. The researchers will finally debrief the participants, to better understand the mechanisms of perception by associating subjective reports with the observed changes.
The researchers have so far found wide variability in participants’ experiences. Some participants report melting and shifting patterns while their eyes are open; others report no visual alterations. Some participants report purely bodily experiences, while others describe accounts of mystical-like journeys. Some participants disclosed a sense of integration, and dissolved separation between themselves and the environment that entailed euphoria; while others experienced these changes with varying emotions.
At this early stage, the research suggests that the quality rather than the intensity of psilocybin experiences may have a greater bearing on psychological changes. Over time, the work hopes to better understand the biological factors that determine the psychedelic response to a given dose, and how mindset and setting can be optimised to aid therapeutic outcomes. Ultimately asking volunteers to take psilocybin for science could help us better understand the brain and how the brain allows us to make sense of ourselves and the world.
If this article has raised issues for you, or if you’re concerned about someone you know, visit Find a helpline for free, confidential support from a real person over phone, text or online chat in your country.
Devon Stoliker is a neuroscientist and consciousness researcher at Monash University, investigating neural connectivity changes under psychedelics and the influence of extra-pharmacological variables on psychedelic experiences and therapeutic outcomes.
Dr Adeel Razi is an Associate Professor, NHMRC Investigator (Emerging Leadership) and Director of the Computational Neuroscience Laboratory at the Turner Institute for Brain and Mental Health and Monash Biomedical Imaging.
The PsiConnect trial is funded by following grants awarded to A/Prof Adeel Razi: CIFAR Azrieli Global Scholar Fellowship, Turner Institute’s Strategic Grant, and Monash Academic Supports Fund.
The authors declare no conflict of interest.
This article has been republished following the Australian Therapeutic Goods Administration (TGA) announcement that from July 1 this year, medicines containing the psychedelic substances psilocybin (found in magic mushrooms) and MDMA can be prescribed by authorised psychiatrists for mental health treatment. It was first published on October 10, 2022.
Originally published under Creative Commons by 360info™.