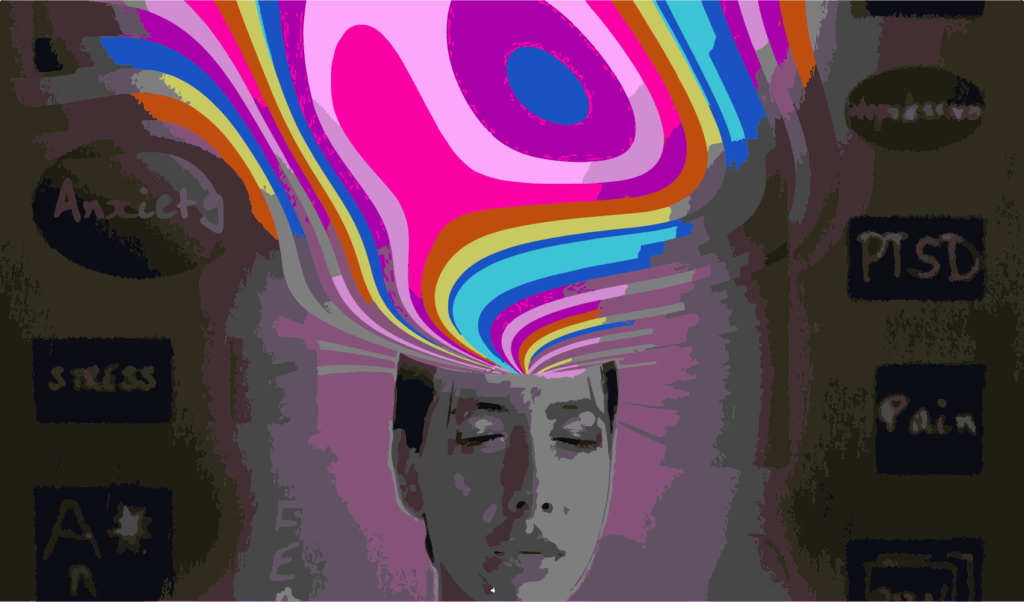
Psychedelic therapies have the potential to treat mental illness but there's still a long way to go.
 Psychedelic therapies involve a specialised form of psychotherapy. : Nik Shuliahin/Unsplash Unsplash license
Psychedelic therapies involve a specialised form of psychotherapy. : Nik Shuliahin/Unsplash Unsplash license
Psychedelic therapies have the potential to treat mental illness but there’s still a long way to go.
After decades in the wilderness, psychedelic therapies are making a comeback into clinical research and are poised to re-enter medical care. When used alongside psychotherapy, drugs like psilocybin (found in ‘magic mushrooms’) and MDMA (found in ‘ecstasy’) have shown large, rapid and sustained benefits for a range of addiction and mental health conditions, including post-traumatic stress disorder, depression, end-of-life distress, alcohol use disorder, and nicotine dependence. While there are some important research limitations associated with these studies, the results have been compelling.
The field of psychedelic research has rapidly expanded, funding is flowing, and public and political sentiment has swung from being largely alarmist or dismissive about these drugs, to hopeful and sometimes hyped. History has shown that some promising treatments can turn out to be underwhelming, unsafe, unfeasible, or unaffordable, and no psychedelic treatment has yet achieved the minimum level of evidence required to be approved as a new medicine. But this may be about to change, and Australia is hurtling towards the likely availability of psychedelic therapies within the next two years.
Only a few years ago, there was no psychedelic research being conducted in Australia. The first psychedelic study in Australia — psilocybin-assisted therapy for end-of-life distress at St Vincent’s Hospital in Melbourne, was approved in 2019. In 2020, researcher Paul Liknaitzky established Australia’s first clinical psychedelic research Lab at Monash University. In 2023, more than 15 clinical psychedelic trials will be active around the country. And by 2024, there is a reasonable chance that MDMA-assisted therapy will be approved as a treatment for post-traumatic stress disorder in Australia. This rapid emergence of a new type of treatment — notably different from any approved medication — may bring new hope to many people.
But to fulfil the promise of safe, effective and accessible psychedelic therapies, significant challenges need to be addressed.
To date, trials worldwide have used a one-size-fits-all treatment model: typically one to three drug sessions, surrounded by about two to four times as many psychotherapy sessions for two to three months. While standardised interventions are common within clinical science, future psychedelic therapy as a service will need to account for a range of different patient needs to maximise safety and effectiveness. These might include different drug doses and dosing sessions, and different amounts and types of psychotherapy. Yet no study has tested the safety and effectiveness of long-term psychedelic therapy, relapse prevention, or tailored treatment.
To be cautious, and for regulation purposes, trials have had narrow eligibility criteria, meaning trial participants may not be representative of future patients. And while multiple concurrent mental health or addiction conditions are more typical among those seeking help, many trials address only a single isolated condition. New studies that recruit participants with more than one condition are important so evidence can drive better decisions.
Psychedelic therapies involve a specialised form of psychotherapy alongside the use of a psychoactive drug. Future clinical psychedelic services should involve a collaborative care team that can assess the suitability of a patient, prescribe controlled drugs, and provide appropriate care. Screeners, prescribers, therapists and support staff would need to have specialist training in psychedelic practice. Optimal treatment centres would offer a private, comfortable and aesthetically appealing space that also has medical and drug storage capabilities.
However, currently only a very small number of trained professionals in Australia have clinical psychedelic experience, few sites are fit-for-purpose, and there is no consensus yet for what constitutes best-practice standards for training or treatment. Both the safety and effectiveness of psychedelic treatments are likely to depend on a range of factors beyond merely getting a psychedelic drug into someone’s body.
One of the most important of these ‘non-drug factors’ is professional support. For this, thousands of psychologists, psychotherapists, drug prescribers, and healthcare workers will need to be adequately trained. Psychedelic medicine is not without risks and is unusual in its use of an altered state of consciousness alongside psychotherapeutic support to increase contact with fundamental sources of distress. A sensible approach would be for already-qualified and experienced clinicians to be further trained in this specialist treatment. Psychedelic therapists would need to undergo supervised practice with patients, perhaps in a student clinic or under direct mentorship. And therapist competencies may be improved if the clinical team have the opportunity to experience psychedelics with support themselves towards increasing attunement — something currently being tested in Monash’s Clinical Psychedelic Research lab.
If psychedelic treatments work as well as current trials suggest, governments, insurers, and patients will save money compared to available treatments and ongoing healthcare, likely within a few years. But the initial costs of psychedelic treatments are likely to be high, estimated to be around AU$15,000 to AU$20,000 for a standard three-dose treatment course over three months. Without reimbursement from the government and insurers, the cost of treatment would be unaffordable for many who may be suitable and in need of new treatment options. Various approaches to cutting costs without undermining the safety and effectiveness of the treatment need to be explored, alongside robust and real-world economic evaluation.
As is common practice for new therapies, a clinical quality registry would be important to monitor real-world and long-term safety and effectiveness for a large number of Australians. This could take the form of brief monthly surveys for patients receiving a psychedelic treatment, and can monitor symptom change, relapse rates, physical and psychological safety and risk factors, costs and ongoing healthcare use, patients’ needs and complaints, and practitioner needs.
Alongside capacity building and training, future research needs to develop and test service-ready psychedelic therapies, focusing on patients with multiple conditions, expanded eligibility for trials, tailored care, comparisons to front-line treatments, and economic evaluation. Such research would produce more than data, informing standards of care, patient suitability, and reimbursement, towards evidence-based psychedelic therapy as a service.
For psychedelic therapies to mature over the next few years into a set of new treatment options that are useful, safe, and accessible, the psychedelic research field has its work cut out. Future patients deserve nothing less.
Paul Liknaitzky is head of Clinical Psychedelic Research at Monash University, and chief Principal Investigator on a program of psychedelic trials at Monash University. He is a joint research fellow within the Department of Psychiatry (School of Clinical Sciences) and the Turner Institute for Brain and Mental Health (School of Psychological Sciences) at Monash University.
He is a member of the Medical Advisory Board of Incannex Healthcare Ltd with no executive role or equity in the company. He has received research funding from Incannex Healthcare Ltd, Dr Nigel Strauss, and the Multidisciplinary Association for Psychedelic Studies.
This article has been republished following the Australian Therapeutic Goods Administration (TGA) announcement that from July 1 this year, medicines containing the psychedelic substances psilocybin (found in magic mushrooms) and MDMA can be prescribed by authorised psychiatrists for mental health treatment. It was first published on October 10, 2022.
Originally published under Creative Commons by 360info™.