A study has found that cost and access are the main barriers to more people using pre-exposure prophylaxis, or PrEP.
 The PrEP Appeal Study looked at PrEP preferences across the Asia Pacific. : Suzannah Lyons and Michael Joiner, 360info CC BY 4.0
The PrEP Appeal Study looked at PrEP preferences across the Asia Pacific. : Suzannah Lyons and Michael Joiner, 360info CC BY 4.0
A study has found that cost and access are the main barriers to more people using pre-exposure prophylaxis, or PrEP.
The PrEP Appeal Study surveyed more than 17,000 men who have sex with men and 1,200 transgender women across 16 countries in the Asia Pacific.
The countries surveyed included Australia, Cambodia, China, India, Indonesia, Japan, Laos, Malaysia, Myanmar, Nepal, Philippines, Singapore, Taiwan, Thailand and Vietnam.
Transcript
Quotes attributed to research associate Curtis Chan from Kirby Institute, UNSW.
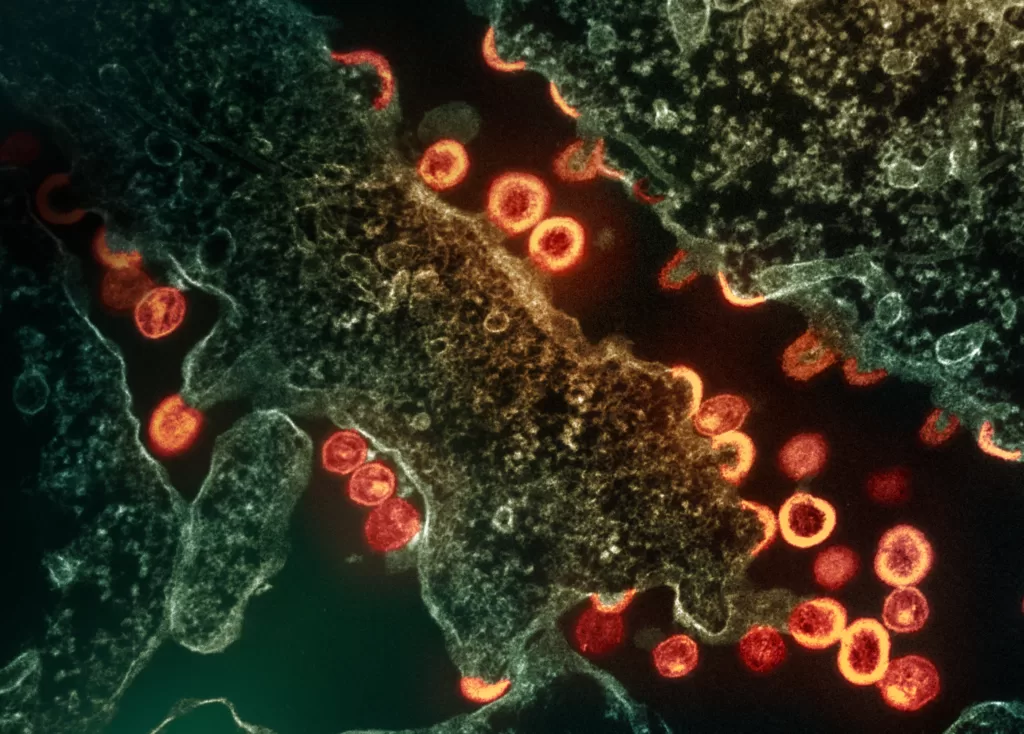
“In the last decade, one of the biggest innovations in HIV prevention is the pre-exposure prophylaxis or PrEP, which is medication that you take to prevent HIV acquisition.”
“So we see that in Australia, we’re at some of the lowest HIV diagnoses in the world, and a lot of that has been attributed to our success in PrEP upscale.”
“But we see that in the Asia-Pacific region there are some of the fastest growing HIV epidemics in the world. Making PrEP more accessible across the region is really important.”
“UNAIDS has set targets for about 4 million people, all in the Asia-Pacific region, to have ever taken PrEP by 2025. But as of 2021, you know, there’s only been about 100,000 who have been estimated to take PrEP. So we are well behind our target.”
“We conducted this survey known as the PrEP APPEAL Study, where we looked at over 17,000 men who have sex with men and 1,200 or so transgender women, and we asked them what they knew about PrEP and what they wanted out of PrEP.”
“So in some countries like Australia, Thailand and Vietnam, you can just go down to the local pharmacy and get PrEP. But in reality, in most of the countries that we surveyed, PrEP is not readily accessible.”
“In some countries you’d have to import it from overseas at a higher cost. So places like Hong Kong and Japan, that’s usually some of the more common ways of getting PrEP. Some countries have clinical trials and other demonstration projects, which means that people are researching PrEP and they’re giving it for free in that way, but it’s not really incorporated into the regular medical system.”
“One thing we asked is how aware people were of PrEP and we found that a lot of people were very aware of PrEP, but of the people who were aware, very few people had actually ever taken PrEP. So about 20 to 30 percent of the men in our survey in Asia had ever taken PrEP, compared to about 66 percent of our Australian respondents. So there was a big divide there.”
“So of the people who had heard of PrEP but had never taken it, about 70 percent said that they wanted to take PrEP, but they commonly cited that not knowing where to get it as well as cost were important factors on why they didn’t initiate PrEP.”
“When we surveyed individual countries, we found that India had a very low PrEP experience. Close to 90 percent of people had never taken PrEP in their lifetime, compared to somewhere like Australia 30 to 40 percent of people said that they’d never taken PrEP.”
“We know that people in places like Taiwan, Hong Kong really liked event-driven dosing. When PrEP was first endorsed by the WHO, it was kind of conceptualised as a daily medication. But we since now know that an effective way of preventing HIV amongst cisgendered men who have sex with men is using what’s known as event-driven dosing. So that means that you can take pills around the time of sex known as on-demand PrEP or 2-1-1 PrEP.”
“You could theoretically get PrEP in Hong Kong and Taiwan because it’s actually not subsidised by the government, it is at a very high cost. And you can import it from other countries overseas.”
“If you have to spend money to get PrEP in a different country, you might want to think a bit more carefully of when you want to take your PrEP and event-driven dosing really suits that kind of dosing strategy.”
“One of the big points of this study was we wanted to know what people thought about hypothetical PrEP options as well as options that were currently available.”
“Some people preferred daily PrEP, some people preferred event-driven PrEP, some people were interested in the new two-month injection known as cabotegravir. But we also know that there’s a large proportion of people that would be interested in taking a six-month injection, a pill that you only take once a month, a removable implant and other options. And so in the future, a big challenge for PrEP implementation is making sure that people have choices available to them.”
“So to make PrEP more accessible, we need more advocacy in this space. So we need more information of what people want, how people want to take PrEP and take it to the governmental bodies in each country and lobby for PrEP uptake.”
“When we think about choice and PrEP implementation, we have to understand that it’s not a one size fits all. What works for Australia might not work for Cambodia, which might not work for Myanmar, and thinking about what each country’s strengths are and what they want from their PrEP implementation is really important.”
“We hope that studies like ours can guide the future of PrEP implementation and bring us one step closer to ending HIV through greater PrEP access.”
Curtis Chan is a research associate and PhD student in HIV prevention at the Kirby Institute, UNSW. You can find him on TikTok @curtisxchan.
Originally published under Creative Commons by 360info™.
Editors Note: In the story “Still fighting HIV” sent at: 30/11/2023 06:00.
This is a corrected repeat.